In the intricate world of healthcare, managing finances is as crucial as providing quality patient care. One of the fundamental aspects of healthcare finance is the healthcare revenue cycle management a process that ensures healthcare providers are reimbursed for their services. Healthcare businesses must comprehend this cycle in order to preserve their financial stability and keep providing top-notch treatment.
What is Healthcare Revenue Cycle?
The Revenue Cycle Management Solutions is the process by which a healthcare provider receives payment for services rendered encompassing everything from patient registration to final payment. It involves a series of steps including patient registration, insurance verification charge capture, claim filing, payment posting and account settlement. Effective management of this cycle is crucial for the financial stability of healthcare facilities.
Key Steps in the Healthcare Revenue Cycle
1. Pre-Registration
- Collecting Patient Information
Prior to a patient visit health care practitioners gather information about patients that includes personal information medical histories and insurance coverage. The verification process lays the groundwork for accurate billing and appropriate delivery of care.
- Insurance Verification
The verification process ultimately confirms the patient’s insurance coverage status, and, therefore, enables the health care practitioner to be cognizant of billed services that would not be covered during the visit. This process will allow the health care practitioner to carefully disclose coverage to the patient, and communicate any financial obligation on the part of the patient. It is in everyone’s best interest that verification occurs at the beginning, and prevents unnecessary surprise denials, and unexpected expenses to patients.
2. Registration
- Confirming Patient Details
When you register, the information learned during pre-registration is checked for accuracy and updated when needed. Correct input is vital for successful billing and communication.
- Obtaining Necessary Authorizations
A few procedures may also require prior authorization from insurance carriers. Obtaining required authorization prior to the provision of services will eliminate delays and denials in any payments.
3. Charge Capture
- Healthcare professionals must document everything that was done for the patient during their visit. This documentation serves a purpose; it is necessary for billing and regulatory purposes.
- Once medical coders translate service documentation into codes that follow standards set by content systems, like ICD-10 and CPT codes, the codes will be used to generate claims for payment.
4. Claim Submission
Once coded, claims are prepared and submitted to insurance companies for payment. For maintaing an ultimate cash flow claim submission should be timely and accurate.
5. Remittance Processing
- Receiving Payments from Payers
Insurance companies process the submitted claims and remit payments to healthcare providers. The remittance includes details about the payment and any adjustments made.
- Posting Payments to Accounts
Received payments are posted to the patient’s account, updating the balance and reflecting the amount paid by the insurer.
6. Insurance Follow-Up
- Managing Denials and Rejections
Not all claims are accepted on the first submission. Denied or rejected claims require follow-up to identify issues, correct errors and resubmit for payment.
- Resubmitting Corrected Claims
Corrected claims are resubmitted to insurance companies for reconsideration. Prompt follow-up helps minimize revenue loss.
7. Patient Collections
- Billing Patients for Remaining Balances
Patients may be liable for co-pays, deductibles, or uninsured treatments following insurance payouts. Billing that is prompt and clear guarantees that patients are aware of their financial responsibilities.
- Implementing Payment Plans
Offering flexible payment options, such as installment plans, can improve patient satisfaction and increase the likelihood of collecting outstanding balances.
Challenges in Healthcare Revenue Cycle Management
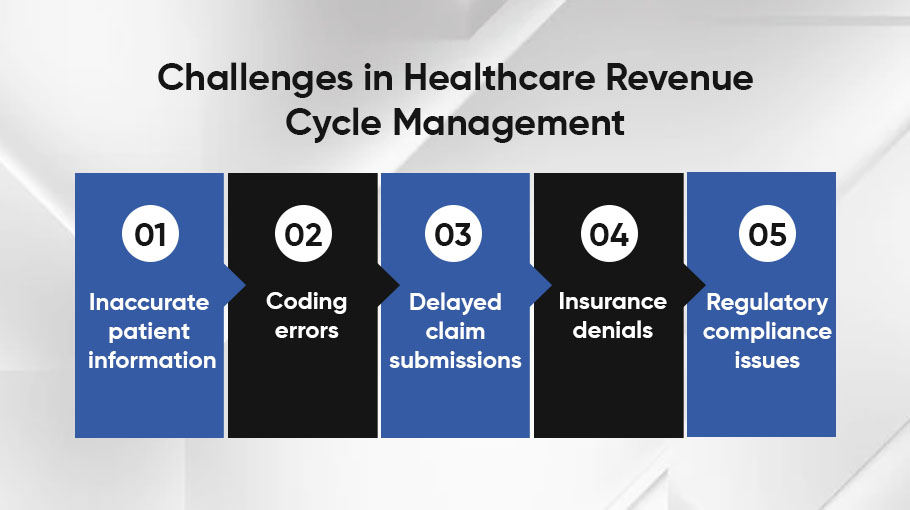
Common Obstacles in RCM
Healthcare providers often face challenges in RCM, including:
- Inaccurate patient information
- Coding errors
- Delayed claim submissions
- Insurance denials
- Regulatory compliance issues
Impact of Errors on Revenue
Revenue cycle errors may result in lower revenue, more administrative expenses, and postponed payments. For financial health, these problems must be resolved quickly.
Managing the Revenue Cycle Effectively
- Implementing Technology Solutions
Utilizing advanced software for billing, coding and claims management can streamline processes, reduce errors and improve efficiency.
- Staff Training and Education
Regular training ensures that staff members are up-to-date with the latest coding standards, billing practices and regulatory requirements.
- Regular Audits and Compliance Checks
Conducting routine audits helps identify areas for improvement, ensure compliance with regulations and prevent potential revenue losses.
Final Thoughts
To guarantee that providers receive payment for their services, healthcare revenue cycle management is an essential part of healthcare operations. Healthcare businesses may improve financial performance, lessen administrative responsibilities, and concentrate on providing high-quality patient care by comprehending and skillfully managing each stage of the revenue cycle.
Leave a Reply